General Information about Avapro
Like any medication, Avapro may work together with other drugs. It is crucial to tell a healthcare supplier of all medicines being taken, together with prescription, over-the-counter, and natural supplements, to avoid potential interactions. Some drugs which will work together with Avapro include diuretics, nonsteroidal anti-inflammatory medication (NSAIDs), and lithium.
As with any treatment, Avapro might trigger side effects in some people. The most typical unwanted facet effects embody dizziness, headache, abdomen upset, and back pain. These symptoms are normally mild and subside with continued use. However, if they persist or turn into bothersome, it is necessary to consult a healthcare supplier. In uncommon cases, extreme side effects such as allergic reactions, liver problems, or kidney failure could happen. It is important to seek medical consideration immediately if any of those signs arise.
Avapro, additionally identified by its generic name irbesartan, is a drugs used to treat hypertension (high blood pressure) and diabetic nephropathy (kidney problems attributable to diabetes). It belongs to a class of medicine often known as angiotensin II receptor antagonists, which work by enjoyable blood vessels and permitting blood to move extra easily, thereby decreasing blood strain.
In addition to treating hypertension, Avapro is also helpful in managing diabetic nephropathy. This condition happens when excessive blood sugar ranges associated with diabetes cause injury to the small blood vessels in the kidneys, impairing their perform. Over time, this could result in kidney failure. Avapro helps to guard the kidneys by decreasing the amount of damage accomplished to those blood vessels and bettering kidney function.
Avapro is not appropriate for everybody. It should not be taken by pregnant girls, as it might hurt the unborn baby. It can be not really helpful for people with a history of angioedema (swelling of the face, lips, throat, or tongue) or those who are allergic to any of the elements within the treatment. It is important to reveal any other medical conditions and medicines being taken to a healthcare provider before starting Avapro.
Hypertension is a condition by which the force of blood in opposition to the walls of the arteries is persistently too high. If left untreated, it might possibly lead to severe well being consequences such as heart attack, stroke, or coronary heart failure. Avapro helps to decrease blood stress by blocking the motion of a hormone referred to as angiotensin II, which constricts blood vessels, causing them to narrow and increase blood strain.
Avapro is available in pill kind and is usually taken as quickly as a day. The dosage might range based mostly on the person's medical situation and response to treatment, so it is essential to observe the prescribed dosage as directed by a healthcare skilled. It may be taken with or without food, but it is strongly recommended to take it on the same time each day to maintain a constant level of the medication in the physique.
In conclusion, Avapro is a extensively used treatment for the therapy of hypertension and diabetic nephropathy. It works by enjoyable blood vessels and enhancing kidney operate, thereby lowering the risk of serious health issues. As with any treatment, it is crucial to comply with the prescribed dosage and seek the assistance of a healthcare provider for any considerations or potential interactions. With correct use, Avapro can help individuals manage their conditions and improve their overall health and well-being.
Failure of caudal neurulation produces a myelomeningocele, whereas more cranial failure results in anencephaly diabetes insipidus bedwetting avapro 300 mg purchase without prescription. One hypothesis is that maternal or fetal mutations in either methionine synthase or 5,10-methylenetetrahydrofolate reductase may slow this "methylation cycle" down, drive the conversion of methionine to homocysteine, and lead to methionine deficiency or homocysteine excess, or both. Ingestion of higher doses of folate may overcome this relative deficiency by restoring more normal homocysteine and methionine levels. Dermal sinuses may involve any level of the neuraxis, although there is a predilection for neuropores in both the lumbosacral and frontonasal regions. Frontonasal dermal sinuses arise through incomplete dysjunction at the site of the anterior neuropore and commonly involve the frontobasal skull. The embryogenesis and surgical anatomy of frontonasal dermal sinuses are predicted by the normal development of the anterior cranial base. A, During normal embryogenesis, the fonticulus nasofrontalis forms between the frontal and nasal bones; the prenasal space forms between the nasal bone and nasal cartilage. B, A tongue of dura extends through the foramen cecum toward the midline nasal skin. Later, this tongue of dura is obliterated and the anterior cranial base is formed; the foramen cecum remains as a vestige of this embryonic tract. C, Abnormal dysjunction during closure of the anterior neuropore leaves a tract of cutaneous ectoderm between the commissural plate and the midline nasal skin. Formation of the anterior frontobasal structures results in a tract whose cutaneous opening may be located at the fonticulus nasofrontalis or anywhere along the dorsum of the nose and that extends through the foramen cecum, between the two halves of a bifid crista galli, and along the anterior cranial base; in rare instances, the tract extends all the way to the commissural plate. Simultaneously, nasal bones develop along the nasal spine and are separated from the frontal bones by a fibrous capsule, the fonticulus nasofrontalis. The nasal spine is separated from the deeper nasal cartilaginous capsule by the prenasal space. During normal embryogenesis, a tongue of dura extends ventrally from the inferior aspect of the anterior cranial fossa and is interposed anteriorly between the frontal and nasal bones at the fonticulus nasofrontalis and inferiorly between the prenasal cartilage and the nasal bones within the prenasal space. During normal development, this dural reflection becomes surrounded by ossifying bone and regresses; remnants of the tract persist as the foramen cecum along the floor of the anterior cranial fossa, between the insertion of the falx cerebri anteriorly and the crista galli posteriorly. When they extend intracranially, they pass through the foramen cecum and typically end within the falx; on rare occasion the tract extends entirely through the falx and travels within the subarachnoid space to end at the lamina terminalis (the site of the anterior neuropore) as predicted embryologically. A malformation involving the cranial rim of the neuropore produces a tract that remains anteriorly located and in close association with the anterior cranial structures. Finally, dermal sinuses are also common in the occipital region,87,88 where they arise from either the roof of the fourth ventricle, the cerebellar vermis, or the subdural space posterior to the cerebellum. The tract may extend either beneath the tentorium into the posterior fossa or above the tentorium toward the occipital lobe or branch to involve both compartments. Although some authors have suggested that occipital dermal sinuses arise from the region of the anterior neuropore,87 this is inconsistent with the association of occipital dermal sinuses with structures derived from the dorsal aspect of the rhombencephalon (cerebellum and fourth ventricle) well distant from the lamina terminalis. Occipital dermal sinuses more likely arise from the rhombencephalic neural tube during neural tube closure. Why dermal sinuses have a predilection for this region of the neuraxis is unclear. The rhombencephalon in humans is among the first regions of the neural tube to undergo neural fold fusion and may therefore be particularly vulnerable to disorders of neurulation; in addition, the presence of the pontine flexure may lend additional physical stress to the neural tube at this site. Finally, the frequent occurrence of dermal sinuses may simply reflect the relatively large size of this region of the neural tube at the time of neurulation. Variably described as the "split notochord syndrome,"89 "endodermal-ectodermal adhesion syndrome,"90 "accessory neurenteric canal syndrome,"91 or "disordered midline integration during gastrulation" syndrome,1 the embryogenesis of these disorders is fully discussed by Dias and Walker. All have in common a splitting of the neuroectoderm into two parts over a portion of its length. Finally, pathologic specimens of both malformations demonstrate neither absolute splitting nor complete duplication of the cord but rather incomplete duplications with relatively well preserved lateral halves and dystrophic medial halves. Beardmore and Wigglesworth101 proposed an adhesion between the epiblast and hypoblast that interferes with notochordal outgrowth. On encountering this "endodermal-ectodermal adhesion," the notochord might split around the adhesion and produce two "heminotochords," each inducing a neural "hemicord. Intracranial Lipomas Lipomas may arise at any level of the neuraxis, although spinal lipomas are the most common and most frequently involve the lumbosacral spinal cord, conus medullaris, and filum terminale. These mesenchymal cells, which are normally induced to form meninx when exposed to the outer surface of the neural tube, are instead induced to form fat on exposure to the central canal of the spinal cord. Intracranial lipomas, in contrast, most likely represent postneurulation abnormalities arising from an abnormality of the meninx primitiva (the anlagen of the pia and arachnoid derived from the cranial neural crest). According to this theory, the meninx primitiva forms initially in what is to become the intracranial cisterns. Maldevelopment of the meninx would therefore least frequently affect those cisterns that develop earlier and most commonly affect those that develop later. Both the preferred anatomic locations, the relationship to (and lipomatous extension into) the choroidal fissure, the passage of cranial nerves through the lipomas, and the maldevelopment of surrounding structures such as the corpus callosum are all predicted by this unifying theory. The primitive streak is abnormally wide (perhaps because of maldevelopment of the underlying basement membrane); prospective notochordal cells therefore begin ingressing more laterally than normal. The caudal neuroepithelium flanking the primitive streak also fails to become integrated to form a single neuroepithelial sheet and instead forms two "hemineural plates. Microcephaly is a common concomitant of encephaloceles; however, it is uncertain whether this is a primary or secondary event. Alternatively, all that may be necessary is a focal area of mesenchymal insufficiency or weakness to allow the rapidly growing telencephalon to herniate; occipital encephaloceles may be produced in chickens simply by incising the occipital mesenchyme overlying the cranial neural tube after neurulation is complete. Some have described all three as part of a continuum of anomalies sharing a common embryologic mechanism. Finally, frontobasal encephaloceles are common in Southeast Asian populations120 and are associated with a number of genetic syndromes,125 whereas frontobasal dermal sinuses, dermoids, and nasal gliomas are not. Disorders of Commissural Connections- Callosal Agenesis Abnormalities of corpus callosum development frequently accompany a variety of other disorders.
Therefore, the dose of induction agents may need to be decreased to minimize cardiovascular depression joslin diabetes diet guidelines 300 mg avapro order mastercard. Etomidate and ketamine are frequently used to induce anesthesia in hemodynamically compromised patients. Finally, preexisting pulmonary dysfunction, as in infants with bronchopulmonary dysplasia or older children with neuromuscular disease, may force delays in extubation because of respiratory insufficiency. In these cases, objective criteria and the presence of an air leak around the endotracheal tube with airway pressures less than 20 to 25 cm H2O will determine the appropriate timing of postoperative extubation. Head-up positioning and gentle forced diuresis usually improve airway edema within 24 hours. Remifentanil is a unique opioid that is rapidly metabolized by plasma esterases and characterized by rapid emergence from anesthesia. Patients receiving chronic anticonvulsant therapy require larger doses of muscle relaxants and narcotics because of induced enzymatic metabolism of these agents. Given the risk for significant blood loss associated with many neurosurgical procedures, a hematocrit and prothrombin time/partial thromboplastin time should be obtained to uncover any insidious hematologic disorders. Small patients have a greater percentage (up to 25%) of their cardiac output directed toward the head. Normal saline is commonly used as the maintenance fluid during neurosurgery because it is mildly hyperosmolar (308 mOsm/kg) and it theoretically attenuates brain edema. However, rapid infusion of a large amount of normal saline (30 mL/kg per hour) is associated with hyperchloremic acidosis. Hyperventilation and careful patient positioning to maximize cerebral venous drainage can minimize brain swelling. This transiently alters cerebral hemodynamics and raises serum osmolality by 10 to 20 mOsm/kg. Furosemide is a useful adjunct to mannitol for decreasing acute cerebral edema and has been shown in vitro to prevent rebound swelling caused by mannitol. Local Anesthesia Neurosurgeons usually infiltrate subcutaneous epinephrine before the surgical incision to minimize cutaneous bleeding. However, all local anesthetics have the potential for cardiac and neurological toxicity. Dilution of bupivacaine with saline can increase the volume of the local anesthetic when necessary and still be effective without increasing toxicity. The Doppler probe is best positioned on the anterior aspect of the chest, usually just to the right of the sternum at the fourth intercostal space. An alternative site on the posterior of the thorax can be used in the prone position for infants weighting approximately 6 kg or less. However, the depressant effects of many anesthetic agents limit the utility of these monitors. A major part of preoperative planning should include a thorough discussion of the modality and type of neurophysiologic monitoring to be used during any surgical procedure. In general, electrocorticography and electroencephalography require low levels of volatile anesthetics and barbiturates. Somatosensory evoked potentials used during spinal and brainstem surgery can be depressed by volatile agents and, to a lesser extent, by nitrous oxide. An opioid-based anesthetic is the most appropriate agent for this type of monitoring. Baseline function should be obtained before surgical manipulation to detect significant deviations during the procedure. Spinal cord and peripheral nerve surgery may require electromyography and detection of muscle movement as an end point. Therefore, muscle relaxation should be avoided or not maintained during the monitoring period. Table 173-9 lists common anesthetic agents and their effects on various neurophysiologic monitors. Central venous catheters are typically inserted for venous access in adult neurosurgical procedures. However, pediatric central venous catheters have a small internal diameter (gauge) and are resistant to high flow rates. Two large peripheral venous cannulas are generally sufficient for most pediatric craniotomies. Use of the femoral vein avoids the risk of pneumothorax associated with subclavian catheters and does not interfere with cerebral venous return, as may be the case with jugular catheters. Furthermore, femoral catheters are more easily accessible to the anesthesiologist during operations on the head. Because significant blood loss and sudden hemodynamic instability can occur during craniotomies, cannulation of an artery provides direct blood pressure monitoring and the ability to obtain frequent blood samples. Monitoring Standard monitoring for all neurosurgical anesthetics includes a stethoscope (precordial or esophageal), electrocardiogram, pulse oximetry, blood pressure, end-tidal carbon dioxide, temperature, and an indwelling bladder catheter. An arterial catheter also provides access for serial sampling of blood for analysis of blood gases, electrolytes, and hematocrit. Central venous pressure may not accurately reflect vascular volume, especially in a child in the prone position. Therefore, the risks associated with a central venous catheter may outweigh its benefits. Standard neurosurgical techniques may elevate the head of the table to improve venous drainage and are conducive to air entrainment into the venous system through open venous channels in bone and sinuses. Patients with cardiac defects, such Thermal Homeostasis Infants and children are especially susceptible to hypothermia during any surgical procedure because of their large surface areato-weight ratio. Active heating of the patient by increasing ambient temperature and use of radiant light warmers during induction of anesthesia, catheter insertion, and preparation and positioning of the patient are prophylactic measures against hypothermia. Mattress warmers, forced hot air blankets, and humidification of inspired gases can also prevent intraoperative temperature loss and postoperative shivering.
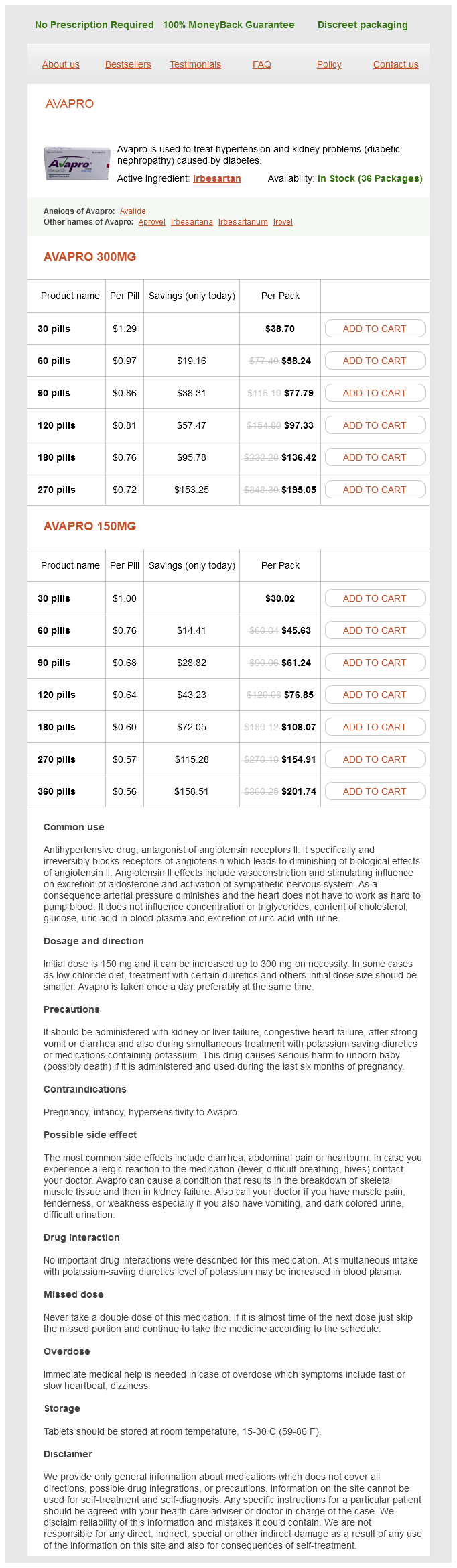
Avapro Dosage and Price
Avapro 300mg
- 30 pills - $38.70
- 60 pills - $58.24
- 90 pills - $77.79
- 120 pills - $97.33
- 180 pills - $136.42
- 270 pills - $195.05
Avapro 150mg
- 30 pills - $30.02
- 60 pills - $45.63
- 90 pills - $61.24
- 120 pills - $76.85
- 180 pills - $108.07
- 270 pills - $154.91
- 360 pills - $201.74
Debris and air bubbles in the shunt valve or catheter will significantly increase turbulence and restrict the diameter of the lumen, both of which will significantly increase resistance to flow; although this does not necessarily occlude the shunt, it may have a major impact on shunt performance blood sugar unit of measure cheap avapro 300 mg buy on-line. The catheters are stiff enough to resist kinking but compliant enough to minimize the risk of brain injury as the ventricles reduce in size and the catheter comes in contact with the ependyma. Most modern catheter designs are impregnated with tantalum or barium to facilitate radiologic identification. The latter is associated with an increased rate of distal shunt catheter deterioration and host reaction leading to calcification and loss of elasticity and strength of the catheter tubing. Packaged catheters carry a static charge and, when opened, can attract airborne dust particles carrying microorganisms; accordingly, nonantibiotic-impregnated catheters should be soaked in sterile saline solution immediately on opening to reduce the risk of contamination. To reduce the risk for shunt infection, manufacturers have introduced specialized catheters, some of which are impregnated with antibiotics, such as the Bactiseal catheter system, which is impregnated with clindamycin and rifampicin (Codman, Johnson & Johnson, Inc. Other manufacturers have developed catheters that are impregnated with silver nanoparticles (Silverline, Speigelberg, Hamburg), which have antibacterial properties,37 or coated with antibiotics to reduce the risk for shunt infection. It should be noted, however, that to date, no prospective multicenter randomized controlled trials have been completed that demonstrate an overall reduction in infection rates with any of these catheters. Some retrospective studies have shown promising results in high-risk populations,38-40 but other series have not demonstrated a benefit,41 and a relative increase in more severe gram-negative infections may offset any benefit from an overall reduction in infection rates. Other measures such as the intraventricular administration of antibiotics at the time of shunt implantation may be of similar efficacy. Occasionally, catheters are placed within the subarachnoid space, arachnoid cysts, syrinx cavities, and subdural hygromas. The most common cause of shunt malfunction is blockage of the proximal catheter, which is usually secondary to ingrowth of choroid plexus. Attempts to identify a preferred site for catheter placement remote from the choroid plexus have been unsuccessful. A variety of proximal catheter designs with baskets, flanges, or recessed holes, as well as the "J"-shaped Hakim catheter with holes on the inside curve of the "J," have been produced in an effort to reduce mechanical obstruction by the choroid plexus, but none have been successful in reducing ventricular catheter blockage rates. Endoscopic coagulation of the choroid plexus itself on the side of the shunt may be the most effective means of reducing proximal catheter obstruction. Laboratory studies have shown that even if only a single hole remains patent, there is no significant increase in the total resistance of the shunt system. A number of devices can be used to facilitate proximal catheter placement, including the Ghajar guide, a tripod designed to ensure a perpendicular trajectory to the ventricle from a coronal approach,47 as well as ultrasound probes and intraluminal ventriculoscopes. Recently, frameless, image-guided neuronavigation has been used to facilitate catheter placement,49 and the advent of electromagnetic navigation technology has enabled the use of such neuronavigation in infants. A variety of rigid connectors (either polyethylene or titanium) are available, either straight, right angled, or "Y," "X," or "T" shaped to facilitate the assembly of complex shunt systems. The latter is associated with a significantly lower rate of distal catheter occlusion,51 and we advocate removal of any distal slits before intraperitoneal placement. When the distal catheter is placed in the vascular system, a distal slit valve is required. This may be useful when cosmesis is a major consideration or when coexistent intra-abdominal pathology such as adhesions or obesity may compromise optimal placement, and it allows confirmation of the implanted functioning shunt system. A new valve design may solve one problem, but only at the expense of another and with no net reduction in shunt-related morbidity. Valve types may be categorized by their mechanism of action: differential pressure valves, which open when the differential pressure of the fluid across the valve exceeds the opening pressure of the valve; flow-controlled valves; and gravitational (gravity-actuated) valves. Devices intended to reduce siphoning are also available as either separate components or integrated into the valve design itself. Valves may have proximal and distal occluders to facilitate percutaneous flushing of the valve, in vivo testing, or drug administration. The valve is composed of a contoured synthetic ruby flow control pin that fits inside a movable synthetic ruby ring. These devices produce pressure-flow curves with a sigmoid shape; at low pressures the valve behaves as a differential pressure valve until flow rates reach about 20 mL/hr. As the pressure increases, the ruby ring is deflected downward, and because the ruby pin is tapered, the flow aperture decreases, which increases resistance and reduces flow. This will tend to maintain flow at a constant level over a range of physiologic pressures (8 to 35 cm H2O). At this point the valve behaves as a differential pressure valve and gives rise to a sigmoid curve. A randomized controlled trial failed to demonstrate a reduction in revision rates with flowcontrolled valves when compared with other conventional differential pressure valve types. Hysteresis occurs because of a slight change in the mechanical properties of the valves, depending on whether they are opening or closing, and occurs most frequently with silicone slit and miter valves. It can have a significant impact on valve performance and potentially lead to overdrainage, even in the absence of siphoning. Unfortunately, there is no industry standard, and the exact pressure characteristics vary considerably between manufacturers. Some manufacturers classify valves according to closing pressure and others according to pressure at a particular flow rate. Most differential pressure valves will allow flow rates far in excess of what would be considered physiologic. Opening pressure is not everything, however; as shown earlier, two different differential pressure valves may have the same opening pressure but completely different resistance values and therefore behave differently. Slit valves may be placed at the proximal end (Holter-Hausner valve) or at the distal end (Codman Unishunt) of a shunt.