General Information about Arcoxia
One of the principle uses of Arcoxia is for the remedy of osteoarthritis, which is a common form of arthritis that impacts tens of millions of individuals worldwide. Osteoarthritis is a degenerative joint disease that causes ache and stiffness in the joints, particularly within the knees, hips, and arms. It is usually attributable to wear and tear on the cartilage (the protecting tissue that cushions the ends of bones) and might result in inflammation and swelling. Arcoxia helps to minimize back these symptoms, making it simpler for individuals to carry out their day by day actions and enjoy a greater high quality of life.
Arcoxia is a popular medication used for the treatment of various forms of arthritis and musculoskeletal pain. It is a non-steroidal anti-inflammatory drug (NSAID) that works by lowering irritation and pain within the body. This medication can provide relief for each acute and chronic situations, making it a versatile option for these affected by joint pain and different related points.
In addition, Arcoxia can also be efficient in treating rheumatoid arthritis, which is an autoimmune disorder that causes pain, swelling, and stiffness in the joints. This condition occurs when the immune system attacks the lining of the joints, leading to joint damage and inflammation. Arcoxia helps to relieve these symptoms by blocking the production of sure chemical compounds within the body that cause inflammation and pain.
Not only is Arcoxia effective in treating numerous forms of arthritis, but additionally it is used for the relief of acute and chronic musculoskeletal pain. This contains ache attributable to injuries, surgeries, and other conditions that have an effect on the muscular tissues, joints, and bones. Arcoxia could be prescribed by a physician for short-term ache relief or for long-term administration of chronic ache, relying on the individual's particular needs.
However, like all medication, Arcoxia may cause unwanted effects in some individuals. The most typical side effects embrace headache, dizziness, constipation, and stomach upset. It is essential to consult a well being care provider earlier than taking Arcoxia, as it could interact with certain medications or medical conditions.
Another frequent use for Arcoxia is the management of ankylosing spondylitis, a kind of arthritis that primarily affects the spine. This situation causes ache and stiffness within the decrease back and also can lead to restricted movement and permanent harm to the backbone if left untreated. Arcoxia helps to minimize back the ache and inflammation related to this situation, allowing patients to hold up higher mobility and flexibility.
In conclusion, Arcoxia is a extensively used medicine for the therapy of arthritis, musculoskeletal ache, and other associated situations. Its effectiveness in reducing ache and irritation, in addition to its longer duration of action, make it a preferred choice for patients on the lookout for relief from their symptoms. However, it is important to solely take this medicine as directed by a doctor and to report any unwanted effects which will occur. With proper use and monitoring, Arcoxia is usually a helpful tool in managing pain and bettering high quality of life for these affected by arthritis and musculoskeletal points.
One main good factor about using Arcoxia is its capacity to offer aid for different types of ache and inflammation within the physique. Unlike some other ache drugs, Arcoxia is well-tolerated by most people and has a decrease risk of gastrointestinal unwanted aspect effects. It also has an extended period of motion, which means that it could provide aid for as much as 24 hours after taking a single dose.
These indications apply to adults as well as to children aged 217 shoes for arthritis in feet and knees discount generic arcoxia uk, in whom treatment may be considered at reduced weightbased doses (see product inserts). Patients with cirrhosis can respond and should not be excluded as candidates for therapy. A pretreatment liver biopsy to assess histologic grade and stage provides substantial information about progression of hepatitis C in the past, has prognostic value for future progression, and can identify such histologic factors as steatosis and stage of fibrosis, which can influence responsiveness to therapy. As therapy has improved for patients with a broad range of histologic severity, and as noninvasive laboratory markers and imaging correlates of fibrosis have gained popularity, some authorities, especially in Europe, have 420 placed less value on, and do not recommend, pretreatment liver biopsies. On the other hand, serum markers of fibrosis are not considered sufficiently accurate, and histologic findings provide important prognostic information to physician and patient. After liver transplantation for end-stage liver disease caused by hepatitis C, recurrent hepatitis C is the rule, and the pace of disease progression is more accelerated than in immunocompetent patients (Chap. An alternative recommendation for ribavirin doses was issued by a European Consensus Conference and consisted of standard, weight-based 10001200 mg for genotypes 1 and 4, but 800 mg for genotypes 2 and 3. Patients with a history of injection-drug use and alcoholism can be treated successfully for chronic hepatitis C, preferably in conjunction with drug- and alcoholtreatment programs. Because ribavirin is excreted renally, patients with end-stage renal disease, including those undergoing dialysis (which does not clear ribavirin), are not ideal candidates for ribavirin therapy. Rare reports suggest that reduced-dose ribavirin can be used, but the frequency of anemia is very high and data on efficacy are limited. Neither the optimal regimen nor the efficacy of therapy is well established in this population. Two protease inhibitors that are in late stages of development, are expected to be approved in 2011. Although these new drugs add elements of additional toxicity (severe rash in 5% of telaprevir-treated patients and anemia in half of boceprevir-treated patients), they represent an opportunity for curing a substantially larger proportion of patients with shorter treatment courses. Cases in which hepatotropic viruses, metabolic/genetic derangements, and hepatotoxic drugs have been excluded represent a spectrum of heterogeneous liver disorders of unknown cause, a proportion of which are most likely autoimmune hepatitis. In all likelihood, predisposition to autoimmunity is inherited, while the liver specificity of this injury is triggered by environmental. For example, patients have been described in whom apparently self-limited cases of acute hepatitis A, B, or C led to autoimmune hepatitis, presumably because of genetic susceptibility or predisposition. In vitro studies have suggested that in patients with this disorder, lymphocytes are capable of becoming sensitized to hepatocyte membrane proteins and of destroying liver cells. Chronic Hepatitis autoimmune hepatitis definition Autoimmune hepatitis is a chronic disorder characterized by continuing hepatocellular necrosis and inflammation, usually with fibrosis, which can progress to cirrhosis and liver failure. Based on contemporary estimates of the natural history of treated autoimmune hepatitis, the 10-year survival is 8090%. The prominence of extrahepatic features of autoimmunity as well as seroimmunologic abnormalities in this disorder supports an autoimmune process in its pathogenesis; this concept is reflected in the labels lupoid, plasma cell, or autoimmune hepatitis. Autoantibodies and other typical features of autoimmunity, however, do not occur in all cases; among 422 Intriguing clues in to the pathogenesis of autoimmune hepatitis come from the observation that circulating autoantibodies are prevalent in patients with this disorder. Arthralgias, arthritis, cutaneous vasculitis, and glomerulonephritis occurring in patients with autoimmune hepatitis appear to be mediated by the deposition of circulating immune complexes in affected tissue vessels, followed by complement activation, inflammation, and tissue injury. Such severe disease accounts for only 20% of cases; the natural history of milder disease is variable, often accentuated by spontaneous remissions and exacerbations. Especially poor prognostic signs include the presence histologically of multilobular collapse at the time of initial presentation and failure of the bilirubin to improve after 2 weeks of therapy. Death may result from hepatic failure, hepatic coma, other complications of cirrhosis. Laboratory features of autoimmune hepatitis are similar to those seen in chronic viral hepatitis. Many patients with autoimmune hepatitis have normal serum bilirubin, alkaline phosphatase, and globulin levels with only minimal aminotransferase elevations. In severe cases, the serum bilirubin level is moderately elevated [51171 mol/L (310 mg/dL)]. The prothrombin time is often prolonged, particularly late in the disease or during active phases. Smoothmuscle antibodies are less specific, seen just as frequently in chronic viral hepatitis. Because of the high levels of globulins achieved in the circulation of some patients with autoimmune hepatitis, occasionally the globulins may bind nonspecifically in solid-phase binding immunoassays for viral antibodies. In fact, studies of autoantibodies in autoimmune hepatitis have led to the recognition of new categories of autoimmune hepatitis. Most of these patients are women and have clinical features similar to , perhaps more severe than, those of patients with type I autoimmune hepatitis. Necroinflammatory activity characterizes the lobular parenchyma, and evidence of hepatocellular regeneration is reflected by "rosette" formation, the occurrence of thickened liver cell plates, and regenerative "pseudolobules. Bile duct injury and granulomas are uncommon; however, a subgroup of patients with autoimmune hepatitis has histologic, biochemical, and serologic features overlapping those of primary biliary cirrhosis (Chap. In this age group, serum ceruloplasmin and serum and urinary copper determinations plus measurement of liver copper levels will establish the correct diagnosis. Furthermore, the presence of extrahepatic features such as arthritis, cutaneous vasculitis, or pleuritis-not to mention the presence of circulating autoantibodies-may cause confusion with rheumatologic disorders such as rheumatoid arthritis and systemic lupus erythematosus. Chronic Hepatitis diagnostiC Criteria An international group has suggested a set of criteria for establishing a diagnosis of autoimmune hepatitis.
Third Part Its course represents in the interior of the bladder wall which extends upwards and laterally from the corresponding ureteric orifice arthritis mutilans order discount arcoxia on-line. Venous Drainage the veins corresponds to the arteries drains in to renal, gonadal and internal iliac veins. Referred pain: the ureteric pain may referred to lumbar region, hypogastric region, external genitalia, testis or tip of the penis in male and labium majus in female due to the same segmental nerve supply from (T11 to L2). The ureteric stone can be removed with a nephroscope inserted through a small incision or by lithotripsy by which focuses a shockwave through the body that breaks the stone in to small pieces then passes with the urine. Impaction of ureteric stone: the ureteric stone commonly impacted in the following constricted areas i. During hysterectomy (surgical omission of uterus) ureter may be involved in the following danger areas. When ureter is cut at upper level: Transplant it in to ileum or sigmoid colon or if cut in a higher level uretero-ureteric anastomosis done. Pain starts at the loin and radiates down to the groin, external genitalia along the segmental supply of the spinal cord (T11 to L2). The renal stone may pass in to the ureter may causing excessive distension of the ureter. It is the continuation of the sigmoid colon at the level of the third sacral vertebra 2. Abdomen and Pelvis 199 Breadth Upper part 4 cm but in lower part it is dilated known as rectal ampulla. Situation It is situated in the posterior part of the true (lesser) pelvis in front of the lower three pieces of sacrum and coccyx. It descends first downwards and backwards, then downwards, and finally downwards and forwards 3. Sacral curve: It is convex backwards which follow the concavity of the sacrum and coccyx. Upper lateral curve: It is convex to the right present at the level of third and fourth sacral vertebrae ii. Middle lateral curve: It is convex to the left, and most prominent present at the level of sacro-coccygeal joint iii. Lower lateral curve: It is convex to the right present at the level of tip of the coccyx. The three lateral curves are rudimentary sacculations affecting the sides of the rectum only 2. Along the concavities of the curves the horizontal rectal valves projects in to the interior of the rectum they support the weight of the feces. The posterior surface of the rectum is entirely devoid of peritoneum Extent Beginning It begins in the median plane as a continuation of sigmoid colon in front of the third sacral vertebra. The rectum ends by continuous with the anal canal at the ano-rectal junction which lies 2 to 3 cm in front of and little below the tip of the coccyx 2. Peculiaritis of the Rectum Although it is a part of the large gut it is devoid of following: 1. Recto-uterine pouch (pouch of Douglas) with its contents (ileum and sigmoid colon). Situation It is situated just above the ampulla, arising from the anterior and right wall just below the level of the anterior peritoneal reflexion. Situated in the lower part of the rectum and disappears when the organ is distended. Middle rectal artery: these are paired branches of anterior division of internal iliac artery. Inferiorly communicates with the external venous plexus by piercing the anal intermuscular septum. It lies between the perianal skin and subcutaneous part or external sphincter muscle c. From the upper part of the plexus about six veins unite to form the trunk of superior rectal vein which drains in to inferior mesenteric vein (portal system). Middle rectal vein arises from each side of the middle of the venous plexus which drains in to the internal iliac vein (systemic vein) f. From the lower part of the venous plexus, the inferior rectal vein drains in to internal pudendal vein (systemic vein). Rectal veins communicates between the tributaries of portal and systematic circulations, 2. As the radicles of superior rectal veins valve less and surrounded by loose areolar tissue, they easily dilated in case of portal hypertension. As the trunk of superior rectal vein pierces the posterior wall of rectum which may be dilated during prolonged straining of defecation in chronic constipation. Lymphatics of the rectum are arranged in intramural and the extramural plexuses 2. These plexuses communicate with the extramural plexus by piercing the rectal wall 4. The lymphatics of extra-mural plexus accompany the blood vessels and are drained as follows. From the upper part: Drains in to left common iliac lymph nodes accompany the middle rectal artery b. From the middle part: Drains in to the internal iliac lymph nodes accompany the superior rectal artery c.
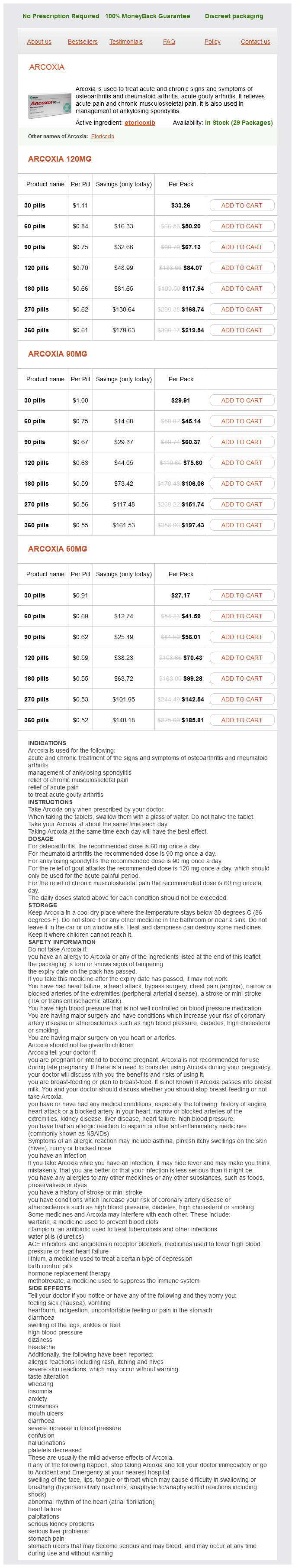
Arcoxia Dosage and Price
Arcoxia 120mg
- 30 pills - $33.26
- 60 pills - $50.20
- 90 pills - $67.13
- 120 pills - $84.07
- 180 pills - $117.94
- 270 pills - $168.74
- 360 pills - $219.54
Arcoxia 90mg
- 30 pills - $29.91
- 60 pills - $45.14
- 90 pills - $60.37
- 120 pills - $75.60
- 180 pills - $106.06
- 270 pills - $151.74
- 360 pills - $197.43
Arcoxia 60mg
- 30 pills - $27.17
- 60 pills - $41.59
- 90 pills - $56.01
- 120 pills - $70.43
- 180 pills - $99.28
- 270 pills - $142.54
- 360 pills - $185.81
In its earliest form arthritis medication during pregnancy order arcoxia 90 mg visa, alcoholic liver disease is marked by fatty infiltration of the liver. In more acute alcoholic hepatitis, there is hepatocyte injury with balloon degeneration and necrosis. However, as in this case, the severe manifestations can include fever, jaundice, spider nevi, and abdominal pain that can mimic an acute abdomen in its severity. Hyperbilirubinemia can be quite marked, with lesser elevation in alkaline phosphatase. The currently preferred agents are octreotide or somatostatin by continuous infusion. Nonspecific beta blockers such as propranolol or nadolol are used for the primary or secondary prevention of variceal bleeding, but are not prescribed in the acute setting as these agents could worsen hypotension. With a sodium restriction to 2 g daily, most mild ascites can be managed quite well. If sodium restriction alone fails to correct ascites, then initiation of diuretics is required. Spironolactone at a dose of 100200 mg daily is the initial diuretic used for ascites and can be titrated as high as 400600 mg daily if tolerated. The typical agent is furosemide beginning at 4080 mg daily with the maximum doses being about 120160 mg daily. Care must be taken to avoid renal dysfunction with loop diuretics, and higher doses may not be tolerated. This procedure creates a portocaval shunt be introducing an expandable metal stent from the hepatic veins through the substance of the liver in to the portal veins, creating a direct portocaval shunt. Although echocardiography is a useful tool for assessing left and right ventricular function, findings may be unimpressive in patients with constrictive pericarditis. Cardiac magnetic resonance imaging may also be helpful in determining which patients should proceed to cardiac surgery. It is characterized by chronic inflammation and fibrous obliteration of intrahepatic ductules. It is associated with lethargy, fatigue, loss of libido, discoloration of the skin, arthralgias, diabetes, and cardiomyopathy. Ferritin levels are usually increased, and the most suggestive laboratory abnormality is an elevated transferrin saturation percentage. Elevated venous pressure leads to congestion of the hepatic sinusoids and of the central vein and centrilobular hepatocytes. Centrilobular fibrosis develops, and fibrosis extends outward from the central vein, not the portal triads. Budd-Chiari syndrome, or occlusion of the hepatic veins or inferior vena cava, may be confused with congestive hepatopathy. However, the signs and symptoms of congestive heart failure are absent in patients with Budd-Chiari syndrome, and these patients can be easily distinguished clinically from those with heart failure. Of these individuals, 3040% with nonalcoholic steatohepatitis will develop advanced fibrosis and 1015% 724 Review and Self-Assessment Ursodeoxycholic acid can be used in some instances to dissolve gallstones. It acts to decrease the cholesterol saturation of bile and also allows the dispersion of cholesterol from stones by producing a lamellar crystalline phase. It is only effective, however, in individuals with radiolucent stones measuring less than 10 mm. Comprehensive testing should include serologies for viral hepatitis, iron studies, ceruloplasmin, 1 antitrypsin levels, and autoimmune serologies. Liver biopsy most commonly shows macrovesicular steatosis with a mixed inflammatory infiltrate in a lobular distribution. The fibrosis that occurs has a characteristic perivenular and perisinusoidal distribution. In cirrhotic patients, steatosis may not be seen, but can recur following transplant. Thiazolidinediones are currently being studied given their effects on insulin resistance. Some predisposing conditions for the development of acalculous cholecystitis include serious trauma or burns, postpartum following prolonged labor, prolonged parenteral hyperalimentation, and the postoperative period following orthopedic and other major surgical procedures. The clinical manifestations of acalculous cholecystitis are identical to calculous disease, but the disease is more difficult to diagnose. In critically ill patients, a percutaneous cholecystostomy may be the safest immediate procedure to decompress an infected gallbladder. Once the patient is stabilized, early elective cholecystectomy should be considered. Metronidazole to provide anaerobic coverage should be added, but this would not elucidate or adequately treat the underlying condition. While the disease is quite prevalent, not all patients with gallstone disease require cholecystectomy. It is estimated that 12% of patients with asymptomatic gallstone disease will develop complications that will require surgery yearly. Therefore, it is important to know which patients with asymptomatic gallstones require referral for surgery. The first factor to consider is whether the patient has symptoms that are caused by gallstones and whether they are frequent enough and severe enough to necessitate surgery.