General Information about Amantadine
Amantadine is a drugs that's widely used for the prevention and therapy of sure forms of flu, including the frequent influenza A virus. However, it's not simply restricted to combating the flu – it is also used within the therapy of Parkinson’s illness and uncontrolled muscle actions brought on by sure medications.
Amantadine is on the market in numerous types, including capsules, tablets, and syrup. It is usually taken once or twice a day, depending on the condition being treated. The dosage and period of treatment could differ primarily based on the individual’s age, medical history, and response to the medication.
Originally developed as an antiviral medicine within the 1960s, amantadine was used to deal with the flu during the outbreak of the Asian flu pandemic. It was later discovered to have useful effects on Parkinson’s disease and became the first medicine approved by the FDA for this condition in 1966.
Amantadine helps to regulate the levels of dopamine within the brain, which may reduce the severity of those movements. It is a well-tolerated and efficient option for managing TD signs, and has been used successfully in combination with different medicines.
Amantadine works by inhibiting the replication of the influenza A virus, making it an effective medication for both prevention and treatment of the flu. It also helps with reducing fever and different flu symptoms, making sufferers feel higher quicker.
The treatment is mostly used as a prophylactic or preventive therapy, especially for people who're at a better danger of contracting the flu, such as healthcare staff or those living in group settings. Studies have proven that amantadine can reduce the incidence of flu by up to 60%.
Amantadine works by stimulating the release of dopamine within the mind, thereby enhancing movement and decreasing tremors. It is usually prescribed together with different drugs for Parkinson’s illness, such as levodopa, to handle symptoms more effectively.
In conclusion, amantadine is a flexible medication that has been proven to be efficient in the prevention and therapy of the flu, as well as in managing symptoms of Parkinson’s illness and TD. Its antiviral properties make it a valuable weapon against the flu, while its capability to stimulate dopamine manufacturing can improve quality of life for people with these conditions. As all the time, you will need to seek the advice of with a healthcare skilled before starting any new treatment.
Furthermore, amantadine has been discovered to be efficient in decreasing the uncontrollable muscle actions brought on by certain medicines, a condition known as tardive dyskinesia (TD). TD can result from long-term use of sure antipsychotic medicines and may cause involuntary actions of the face, tongue, and limbs.
In addition to its antiviral properties, amantadine has also been discovered to have helpful results on Parkinson’s illness. This is a neurodegenerative dysfunction characterized by the loss of brain cells that produce dopamine, a chemical messenger liable for coordinating movement. The signs of Parkinson’s disease include tremors, stiffness, and difficulty with balance and coordination.
As with any medicine, amantadine may trigger unwanted aspect effects in some individuals. Common unwanted side effects include dizziness, headache, dry mouth, and constipation. In rare circumstances, extra severe unwanted effects could occur, similar to coronary heart palpitations, issue urinating, and hallucinations. It is important to consult with a well being care provider if any concerning unwanted effects are skilled.
Blood pressure outcome of angioplasty in atherosclerotic renal artery stenosis: A randomized trial hiv infection rate in africa buy 100 mg amantadine visa. Use of Doppler ultrasonography to predict the outcome of therapy for renal artery stenosis. Factors predicting outcome in a cohort of patients with atheroscleroticrenal artery disease diagnose by magnetic resonance angiography. Efficacy of revascularization for renal artery stenosis caused by fibromuscular dysplasia: A systematic review and meta-analysis. The effect of balloon angioplasty on hypertension inatherosclerotic renal artery stenosis. Randomized comparison of percutaneous angioplasty vs continued medical therapy for hypertensive patients with atheromatous renal artery stenosis. As a result of an autonomously functioning adrenal adenoma, it is called Conn syndrome, after Jerome William Conn (1907 to 1994). More common is bilateral adrenal hyperplasia (sometimes called idiopathic hyperaldosteronism), in which both glands oversecrete aldosterone. Glucocorticoid-remediable hyperaldosteronism results from a chimeric gene on chromosome 8 that crosses the regulatory sequence for corticotropin, 11b-hydroxylase, with the enzyme coding sequences for aldosterone synthase. Hyperaldosteronism from an adrenal carcinoma is rare (30 cases worldwide) and usually presents as a large tumor. Renovascular hypertension is another example of secondary hyperaldosteronism causing hypertension. Some referral centers report a prevalence of hyperaldosteronism related to sleep apnea at about 20%, similar to the original estimate for aldosterone-secreting adenomas proposed by Conn in 1954. Other populationbased studies suggest that such a high prevalence is a result of a lack of specificity of the aldosteronerenin ratio that is often used to screen for the condition. After total body potassium stores have been repleted, the ratio of plasma aldosterone to renin measured in (optimally, untreated) patients in the seated position at 8 am is the most widely recommended test. None of these are perfect discriminators, but the updated 2016 Endocrine Society guidelines suggest usually performing one of these confirmatory tests before imaging the adrenals. Spironolactone had superior efficacy in lowering blood pressure compared to eplerenone in one international clinical trial, but the latter has fewer adverse effects. Strict attention to eukalemia is important, particularly in the first few days after the operation. Most patients receive normal saline, without potassium, during the immediate postoperative period. A day after the procedure, a plasma aldosterone level is measured, potassium supplements and aldosterone antagonists are discontinued, and the patient is counseled to consume more dietary sodium than usual, to minimize the risk of hyperkalemia while the contralateral adrenal gland recovers function. Hyperkalemia is more common in patients with chronic kidney disease (albuminuria, increased serum creatinine, or both). Long-term resolution of hypokalemia is common, but about 50% of patients remain hypertensive (and require antihypertensive medications), even after a successful operation. Persistent hypertension is more common in older patients and those with a longer duration of hypertension before the diagnosis was made. Cushing syndrome is a characteristic set of signs and symptoms resulting from excessive effects of cortisol, initially attributed to a basophilic pituitary adenoma (Cushing disease) by Harvey Cushing in 1932. Cushing syndrome is characterized by progressive physical changes, which are often best appreciated in serial photographs: · Central (truncal) obesity · Moon facies · Dorsocervical fat pad (buffalo hump) · Purple abdominal striae may be the most specific physical sign if. Other features of Cushing syndrome include emotional and cognitive changes, menstrual irregularity, glucose intolerance, and hypertension. Corticotropin-dependent: · Pituitary microadenoma (68% of endogenous hypercortisolemia) · Ectopic corticotropin production (12%, from other tumors, typically small-cell lung cancer) · Ectopic corticotropin-releasing hormone secretion (,1%) Corticotropin-independent: · Exogenous glucocorticoid administration (iatrogenic causes are the most common in the United States) · Adrenal adenoma (10%) · Adrenal adenocarcinoma (8%) · Primary pigmented nodular adrenal hyperplasia (,1%) · McCune-Albright syndrome (,1%) · Macronodular adrenal disease (,1%) · Hyperfunction of adrenal rest tissue (,1%) 1 3. Cushing disease refers to that subset of patients with Cushing syndrome due to a corticotropin-secreting pituitary microadenoma. Many clinicians use the overnight dexamethasone suppression test (which is more convenient than the classical "low-dose" test) as a screen for Cushing syndrome. Classically, the high-dose dexamethasone suppression test (2 mg every 6 hours for eight doses) suppresses the production of cortisol by. A more convenient "high-dose" test measures plasma cortisol at bedtime, followed by one 8 mg dose of dexamethasone and another cortisol level test 8 hours later; "suppression" is diagnosed if the cortisol level drops by 50% compared to baseline. This test does not distinguish between Cushing disease and the far less common ectopic corticotropin secretion, so a chest x-ray is usually scrutinized for evidence of a tumor that is secreting corticotropin. Agents that modulate corticotropin release (cyproheptadine, bromocriptine, valproic acid) or inhibit cortisol synthesis and/or production (mitotane, trilostane, ketoconazole, aminoglutethimide, and metyrapone) may be useful preoperatively or for patients who are not surgical candidates. Testing should be considered for patients with hypertension who present with the characteristic clinical features of Cushing syndrome. The reduction in cortisol synthesis leads to a loss of feedback inhibition of the hypothalamicpituitary-adrenal axis, with excessive production of corticotropin. Exposure to excessive corticotropin leads to adrenal hyperplasia, overproduction of adrenal steroids that do not require the deficient enzyme, and deficiency of steroids distal to the deficient enzyme. Simplified biochemical pathways for steroid biosynthesis (enzymes are given in italics). The specific clinical features depend on the deficient enzyme involved: · Abnormal fetal genital development. Postnatal consequences of this include sex steroid imbalance, including abnormal patterns of growth and maturation, and impaired fertility. Patients with classic 21-hydroxylase deficiency do not have hypertension, but instead have severe salt wasting with dehydration, hyponatremia, and hyperkalemia, which is related to aldosterone deficiency. Abnormal enzyme activity can be manifested as isolated 17a-hydroxylase deficiency, 17,20-lyase deficiency, or their combination.
In normal parturients hiv symptoms of infection amantadine 100 mg order without a prescription, this insult induces a reflex cardiovascular response directed toward maintaining systemic blood pressure. Co-loading of an adequate intravenous crystalloid infusion, keeping the parturient on her side, and minimizing the dose of the local anesthetic all minimize the adverse decrease in blood flow to the pelvis and its structures. High epidural anesthesia that extends to T4 -S5 is associated with a significant interruption of vasomotor segments, resulting in significant hypotension. Again, fluid co-load and lateral tilt of the parturient can augment the reflex corrective responses of the cardiovascular system in this situation. Extending the epidural blockade above spinal level T 10 is unnecessary and counterproductive for the normal laboring patient. If epidural analgesia needs to be changed to anesthesia for a cesarean section, these risks are necessary and measures to prevent them should be instituted In addition, Neo-Synephrine is the best vasopressor to augment blood pressure without reducing blood supply to the uterus. Studies suggest there is improved fetal acid-base status and Apgar scores with prophylactic Neo-Synephrine boluses and infusion as compared to ephedrine as was previously used Contraindications to lumbar epidural analgesia/anesthesia are reviewed in Table 20-5. The advantages and disadvantages of regional analgesia/anesthesia are outlined in Table 20-6. A combined spinal/epidural analgesia technique provides rapid onset of spinal opioid analgesia, plus the flexibility of the epidural blockade. Sufentanil 10 µg or fentanyl 25 µg injected spinally; when the epidural catheter is inserted. Less motor blockade, less hypotension, less local anesthetic administered with inherent toxicity risk, and faster onset of analgesia are all benefits of this combined technique. The side effects of intrathecal opioids and corresponding treatment are listed in Table 20-7. Fetal Bradycardia in Epidural Analgesia and Combined Spinal/Epidural Techniques Fetal bradycardia is a nonreassuring fetal heart rate after induction ofneuraxial anesthesia that may be due to maternal hypotension or uterine hyperactivity. It is mostly associated with the combined spinal/epidural technique but can be seen with any technique that produces profound analgesia. Another proposed explanation is that the fetal bradycardia is due to intrathecal opioid-induced uterine hypertonus. This is followed with decreased placental blood flow, fetal asphyxia, and fetal bradycardia. Preanalgesic adequate hydration of the patient must be achieved with co-loading using crystalloids, as well as, the prevention of overdosing with high blocks beyond that necessary to achieve analgesia for the nerve roots involved with the labor pains. With this physiological understanding of the dynamics occurring, treatment is based on relaxing the uterus. Uterine hypertonus may be reversed with one or two doses of intravenous nitroglycerin (60-90 µg). Persistent hypertonus can be treated with another dose of nitroglycerin or a ~-agonist, such as terbutaline 0. When the patient experiences labor pain, local anesthetic may be injected to achieve a T10·L1 neuroblockade. In late first stage and mid-second stage of labor, the patient should be elevated 15 to 20 degrees to allow caudad spread of local anesthetic to achieve a T10-S15 block. Contraindications to Lumbar Epldural Analgesla/Anesthesla · Parturients who refuse the block or have great fear of puncture of the spine. In our experience, many patients who are concerned initially about epidural block will consent to be managed with this technique provided they are properly informed. However, if they still refuse, it is an absolute contraindication to the technique. Relatlve contraindications Include: · Lack of appreciation by the obstetrician as to how the procedure influences the management of labor. On the other hand, for the anesthesiologist who is very skilled and has had extensive experience, extension of the epidural block in patients who have had the catheter in place during labor can be done as rapidly as getting things ready for anesthesia. Advantages and Disadvantages of Reglonal Analgesla/Anesthesla Advantages · In contrast to opioids, regional analgesia produces complete relief from pain in most parturients. Disadvantages · Regional techniques require greater skill to administer than do administration of systemic drugs or inhalation agents. Current standards in the United States for management ofwaste anesthetic gases call for no more than 25 ppm. Apoptotic loss of neurons in the brains of newborn rodents exposed to N2 0 also creates concern about exposure of moms and fetuses. However, studies seem to show reversible loss, and damage only occurs in very high concentrations ofN20. The transvaginal approach points the needle behind the sacrospinous ligament aiming toward the ischial spine. Up to 5 mg/kg of lidocaine (I% solution without epinephrine) total dose provides reliefof perinea! Although these techniques are relatively easy to execute, a thorough knowledge of pharmacology, the anatomy, physiology, and effects of these drugs on mother and fetus is paramount. Nitrous Oxide for Labor Analgesla A mixture of inhaled nitrous oxide (Np) 50% and 0 2 50% is used for analgesia in labor in many countries and is now available for use in the United States. It can be administered quickly, and discontinued quickly (completely gone within 5 minut. Concerns Related to N20 Concern about occupational risk from repeated exposure for healthcare providers comes from the action of inactivation of methionine synthase, an enzyme necessary for normal cell function. The needle passes behind the sacrcspinous ligament and posterior to the ischial spine. Aspiration, prior to injection of the local anesthetic drug, Is prudent to avoid Inadvertent lntravascular administration. Using up to 5 mg/kg of Udocaine in a 1% solution total dose will give good pain relief for approximately 2 hours.
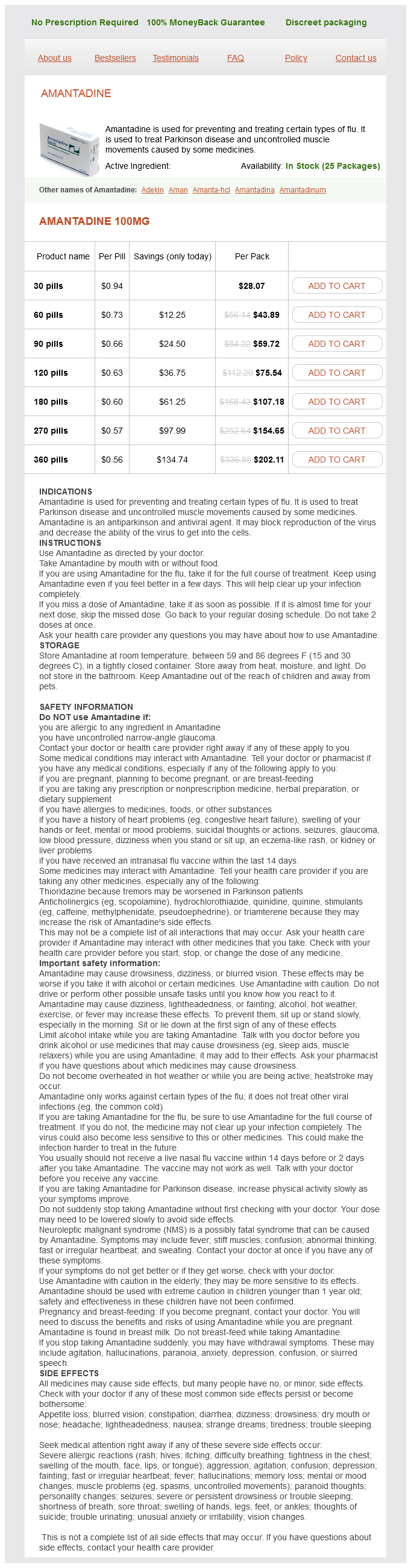
Amantadine Dosage and Price
Amantadine 100mg
- 30 pills - $28.07
- 60 pills - $43.89
- 90 pills - $59.72
- 120 pills - $75.54
- 180 pills - $107.18
- 270 pills - $154.65
- 360 pills - $202.11
Many groups have shown that sarcopenia predicts postoperative complications for a broad range of surgical interventions [39À41] antiviral iv for herpes generic amantadine 100 mg. Muscle wasting may be associated with disease-specific outcomes, such as increased susceptibility to chemotherapy toxicities in cancer, postoperative complications for surgery, decreased left ventricular ejection fraction in heart failure patients, and increased encephalopathy for liver cirrhosis. They showed that in pancreatic cancer patients, one-third had an increase in muscle mass, one-third had a stable muscle mass, and one-third had decreased muscle mass, while all but one patient lost adipose tissue. They showed that 60% of patients gained or stabilized muscle mass, notably in patients with long survival, with the majority of cases of muscle gain (84%) occurring at least 3 months before death. These retrospective studies offer important data showing that gaining or maintaining muscle mass is possible for cancer patients and that tumor response is a principal factor in muscle gain. Currently, few studies have evaluated other potential factors which may favor a positive net balance between protein synthesis and protein breakdown. A more recent view suggests that these two biochemical processes are not independent of each other but are in fact precisely coordinated by a web of intricate signaling networks [45,46]. While it has been demonstrated in healthy humans that increasing food and protein intake can stimulate protein synthesis, this is not necessarily the case in catabolic situations. Reduced protein synthetic response to food intake has been termed anabolic resistance. There are also solid data demonstrating the capacity of leucine to modulate protein metabolism by increasing substrate availability, increasing the secretion of anabolic hormones such as insulin, and directly modulating anabolic signaling pathways by stimulating protein synthesis and reducing protein breakdown [49]. Since this study, many others have been published and the mechanisms involved in muscle wasting appear highly complex. Few data are available, obtained from very disparate clinical studies from a wide variety of settings, including both highly sophisticated protein kinetic studies and clinical trials. Six kinetic studies have been published to date, three focusing on global protein turnover [51À53], while three studied muscle protein metabolism from muscle biopsies [54À56]. It is currently difficult to draw conclusions from these protein kinetic data given the small number of studies published. The translation of acute anabolic effects into gains in muscle mass and function need to be confirmed by long-term intervention trials. An overview of the six studies assessing whole-body protein synthesis and whole-body protein balance is provided below. This study demonstrated that whole-body protein turnover is higher in cancer patients than in controls. Both groups generated a similar anabolic response to feeding; cancer patients achieved this by reducing protein breakdown, whereas controls increased their protein synthesis. The increase in whole-body protein turnover could be associated with a reprioritization of nitrogen away from peripheral tissue (muscle) toward increased hepatic production of acute phase proteins, as described in 1978 by Lundholm et al. Interestingly, these patients were still receiving chemotherapy and were not in a terminal stage of their cancer. They studied patients before and after tumor resection and compared them with a healthy agematched control group. Despite the differences in the results of these six studies, a number of general conclusions can again be drawn: 1. Early in tumor evolution with low or normal protein intake, there is a decrease in muscle protein anabolism (two of the three studies with muscle biopsies). Of note, anabolic resistance was observed early with or without very low weight loss (about 2%). Interestingly, patients in most of the studies had low inflammatory systemic syndrome. Energy intake was normal in all three studies where this information was available which may reflect that patients were at an early disease stage. With increasing protein intake, irrespective of whether or not it contained leucine, five of the six studies showed the potential for increasing the net protein balance, including the three studies that explored whole protein turnover and two of the three studies that explored the fractional synthetic rate in muscle biopsies. An important point that should be highlighted is that in both of these studies, many patients withdrew before the end of the protocol. The lack of benefit of the nutritional support could be related to the status of disease progression, and the treated patients could have been in a refractory cachexia setting where nutritional support is pointless. Despite the potential beneficial results, the role of specific nutriment supplementation remains to be clarified given the inconsistencies of the findings, patient heterogeneity, small sample size, and the poor study design [58,61,62]. Few human studies, and most conducted in patients undergoing surgery, are available [65,66], so there is currently little evidence to support a beneficial effect of arginine and citrulline as a treatment for muscle wasting. Few studies have focused on the effect of adding leucine alone or in combination with other ingredients to the diet. In addition, improvements were also seen in grip strength and mental health score although not in physical health score [67]. Although in animal models some nutritional interventions can counteract body wasting and muscle loss, there is no evidence of proven effects in humans. Overall, a review of the literature shows that nutritional intervention is probably effective in undernourished patients and the effect is greatest when combined with an exercise program. The considerable heterogeneity of the studies and the fact that most were underpowered does not allow for formulation of any clinical recommendations. Omega-3 fatty acids are well known for their inhibition of the inflammatory process, leading to a decrease in protein breakdown. Few clinical studies with lean body mass or muscle mass assessments have been published in cancer patients. These data suggest that omega-3 fatty acids could potentially counteract anabolic resistance and muscle wasting. However, further research should be performed to define the optimal dose and timing of administration. For cancer patients, muscle wasting is associated with susceptibility to chemotherapy toxicities, worse progression-free and overall survival, and more postoperative complications.